What is ovarian cancer?
Cancer is a disease in which cells
in the body grow out of control.
Cancer is always named for the
part of the body where it starts,
even if it spreads to other body
parts later.
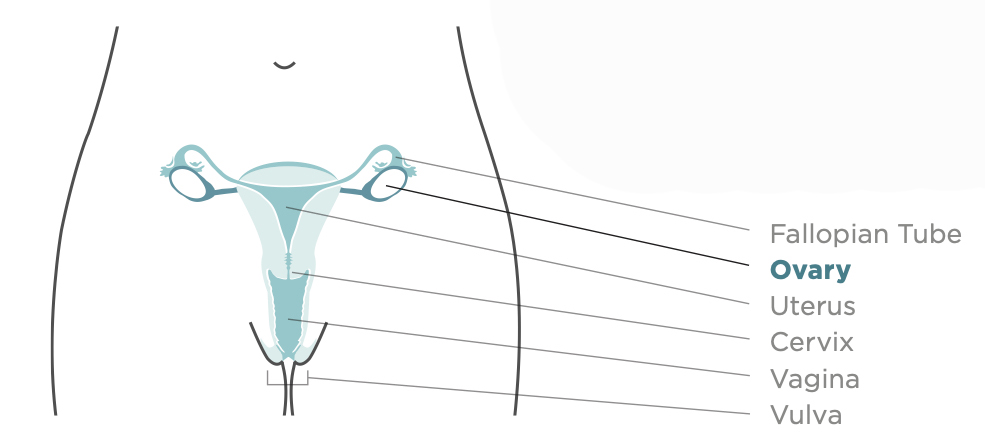
When cancer starts in the ovaries,
it is called ovarian cancer. Women
have two ovaries that are located in
the pelvis, one on each side of the
uterus. The ovaries make female
hormones and produce eggs.
When ovarian cancer is found
in its early stages, treatment is
most effective.
Who gets ovarian cancer?
All women are at risk for ovarian cancer, but older women are more likely to get the disease than younger women. About 90 percent of women who get ovarian cancer are older than 40, with the greatest number of ovarian cancers occurring in women aged 60 years or older. Each year, approximately 21,000 women in the United States get ovarian cancer. Among women in the United States, ovarian cancer is the eighth most common cancer and the fifth leading cause of cancer death.
What raises a woman's chance of getting ovarian cancer?
There is no way to know for sure if you will get ovarian cancer. Most women who get it don't have a family history of ovarian cancer. However, the following factors may increase a woman's risk for ovarian cancer:
• Being middle-aged or older
• Having close family members (such as our mother, sister, aunt, or grandmother) on either your mother's or your father's side who have had ovarian cancer.
• Having had breast, uterine, or colorectal cancer
• Having an Eastern European(Ashkenazi) Jewish background
• Having never given birth or having had trouble getting pregnant
• Having endometriosis (a condition where tissue from the lining of the uterus grows elsewhere in the body).
If you have one or more of these factors, it does not mean you will get ovarian cancer. But you should speak with your doctor or other health professional about your risk.
What are the signs and symptoms of ovarian cancer?
Ovarian cancer may cause one or more of these signs and symptoms:
• Vaginal bleeding (particularly if you are past menopause) or discharge from your vagina that is not normal for you.
• Pain or pressure in the pelvic or abdominal area (the area below your stomach and in between your hip bones).
• Back pain.
• Bloating, which is when the area below your stomach swells or feels full.
• Feeling full too quickly or difficulty eating.
• A change in your bathroom habits, such as more frequent or urgent need to urinate and/or constipation.
Pay attention to your body, and know what is normal for you.
If you have vaginal bleeding that is not normal for you, see a doctor right away. If you have any of the other signs for two
weeks or longer, see a doctor.
These symptoms may be caused by something other than cancer, but the only way to know is to see your doctor. Treatment is most effective when ovarian cancer is found and treated early.
How can I prevent ovarian cancer?
There is no known way to prevent ovarian cancer*. But these things may lower your chance of getting ovarian cancer:
• Having used birth control pills for more than five years.
• Having given birth.
• Having had a tubal ligation (getting your tubes tied),both ovaries removed, or hysterectomy (an operation in which the uterus,
and sometimes the cervix, is removed).
• Breastfeeding. Some studies suggest that women who breastfeed for a year or more may have a modestly reduced risk of
ovarian cancer.
Are there tests that can find ovarian cancer early?
There is no simple and reliable way to test for ovarian cancer in women who do not have any signs or symptoms. The Pap test does not screen for ovarian cancer. The only cancer the Pap test screens for is cervical cancer.
However, here are steps you can take:
• Pay attention to your body, and know what is normal for you. If you notice any changes in your body that are not normal
for you and could be a sign of ovarian cancer, talk to your doctor and ask about possible causes, such as ovarian cancer.
Ask your doctor if you should have a test, such as a rectovaginal pelvic exam, a transvaginal ultrasound, or a CA-125 blood test
if:
You have any unexplained signs or symptoms of ovarian cancer. These tests sometimes help find or rule out ovarian cancer.
You have had breast, uterine or colorectal cancer: or a close relative has had ovarian cancer.
What should I do if my doctor says I have ovarian cancer?
If your doctor says that you have ovarian cancer, ask to be referred to a gynecologic oncologist-a doctor who has been trained to treat cancers like this. This doctor will work with you to create a treatment plan.
- An article published on February 2nd in The Washington Post highlights a turning point in our fight against ovarian cancer.

As covered in the article, “Fallopian tube removal advised for more women to prevent ovarian cancer,” OCRA released a consensus statement, endorsed by the Society of Gynecologic Oncology, encouraging an aggressive prevention strategy: removal of the fallopian tubes while undergoing pelvic surgery for another reason.
The Washington Post writes, “The guidance to remove [fallopian tubes] … is not entirely new — it reflects conversations many doctors already have with their patients and mirrors guidelines from at least two medical groups. But the advice is certain to draw increased attention to fallopian tube removal as a way to lower ovarian cancer risk.”
“I can guarantee you these conversations happen,” said Arif Kamal, chief patient officer for the American Cancer Society. “This is now an important group that has come out and said ‘We really do think these conversations should happen pretty regularly.’”
Ovarian Cancer Research Alliance, a leading cancer research group, recently posted a consensus statement encouraging patients to consider preventive fallopian tube removal if they are undergoing pelvic surgery for another noncancerous condition including hysterectomy, tubal ligations, cysts and endometriosis.
The group notes that because “the fallopian tube is the origin of most high-grade serous cancers, fallopian tube removal has been shown to dramatically reduce risk for a later ovarian cancer diagnosis.”
The group’s recommendations, first reported in The New York Times, also encourage women and anyone born with ovaries to learn more about their genetic risk for ovarian cancer.
Efforts to identify a screening test for ovarian cancer have failed. A large British clinical trial used scans and blood tests hoping to find ovarian cancer at an early stage, but the results showed the screening tests didn’t reduce deaths from the disease.
“We knew it was an important study. We knew that we needed to change the dialogue because we’re the largest ovarian cancer organization in the world and we had a responsibility,” said Audra Moran, president and chief executive of Ovarian Cancer Research Alliance, or OCRA.